INTRODUCTION:
Acute promyelocytic leukemia (APL) accounts for 5-8% of all cases of acute myeloid leukemia (AML). The combination of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO) without chemotherapy is currently the reference treatment of standard APL (ie with baseline white blood count (WBC)<10 G/L), curing about 90% of the patients. However, the prognosis of high-risk APL (ie with WBC>10 G/L) remains more challenging, with higher rates of early death and relapse.
Here we compared the French practices for the treatment of high-risk APL patients whether patients were treated with ATRA-Chemo or ATRA-ATO according to physician decision, and evaluate the response rates, overall survival (OS) and leukemia-free survival (LFS) in the real-life settings.
PATIENTS AND METHODS:
ATO (in combination with ATRA) became accessible in France for the first line treatment of standard risk APL in 2012, but some patients with high-risk APL also received the same combination (generally with some form of cytoreductive chemotherapy) from that date. We retrospectively analyzed cases of high-risk APL diagnosed between 2010 and 2021 in 12 French centers, constituting a cohort of 135 patients with diagnostic of APL confirmed by cytogenetic, FISH and molecular biology assays.
RESULTS:
Among the 135 patients with WBC>10 G/L, 88 (65%) were classified as APL variant according to FAB classification. Median age was 46 years (range 18-89) and 62 % were male. Median diagnostic WBC was 39.1 G/L (range 10-270) and median platelet count was 27 G/L (range 5-344). At diagnosis, 112 patients (83%) had hemorrhagic manifestations and disseminated intravascular coagulation (DIC) was observed in 124 patients (92%). Pulmonary and cerebral leucostasis were reported in 10 (7%) and 14 (10%) patients, respectively. Eighty-five patients received corticosteroid prophylaxis (81 (95%) with Dexamethasone and 5 (5%) with Prednisolone).
Induction therapy consisted in ATRA-ATO for 50 patients (38%) while 85 patients (62%) were treated with ATRA combined with chemotherapy (anthracycline and cytarabin) but without ATO. All patients treated with ATO were cytoreduced: 7 with Hydroxyurea (14%), 17 with Idarubicin (34%) and 26 with both (52%). 29 patients treated without ATO during induction were cytoreduced with Hydroxurea (34%).
Most patients experienced one or more adverse events during induction, including sepsis (49 in the ATO group versus 71 in the non ATO group, 98% versus 83.5%, p=0.01), differentiation syndrome (20 in the ATO group versus 27 in the non ATO group, 40% versus 31.7%, p=0.33), transaminase increased (14 in ATO group versus 11 in the non ATO group, 28% versus 12.9%, p=0.03), and bleeding (7 in the ATO group versus 13 in the non ATO group, 14% versus 15.3%, p=0.8).
Following induction, 110 patients (81%) achieved complete remission (CR): 45 in the ATO group and 65 in the non ATO group (90% versus 76.4%, p=0.052). One patient (receiving ATRA with chemotherapy) was refractory, and 24 patients experienced early death (5 in the ATO group and 19 in the non ATO group, 10% versus 22.3%, p=0.069) mostly due to hemorrhage or sepsis. Median time between diagnosis and early death was 4.5 days (0-42). Relapse was observed in 6 (5.5 %) patients (5 patients treated without ATO and 1 patient with ATO during induction).
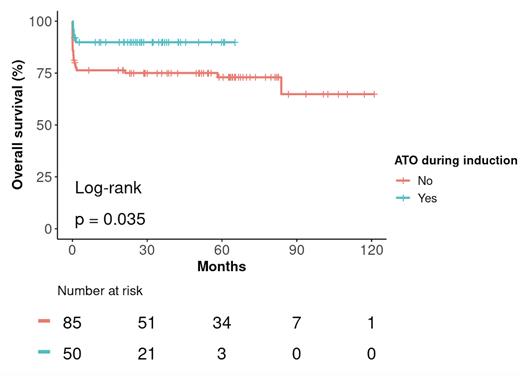
After a median follow-up of 34.6 months (0-121.1), OS at 3 years was significantly higher for the ATO group (89.9% (81.8-98.7) versus 75.1% (66.3-84.9) for the non ATO group, p= 0.035, Figure). LFS at 3 years was significantly higher for the ATO group (87.6% (78.7-97.4) versus 71.2% (62-81.7) for the non ATO group, p=0.028).
CONCLUSIONS:
The survival outcomes were significantly poorer in high-risk APL patients treated without ATO during induction, regardless of the cytoreduction strategy. The toxicity profile of ATO was acceptable. Combining ATO and ATRA limits the use of cytotoxic chemotherapy, which could reduce myelosuppression and long-term complications such as cardiotoxicity and secondary myeloid neoplasms. Early disease-related mortality, due to haemorrhagic or infectious complications, remains the major issue for these patients but tend to be reduced in those receiving ATRA-ATO based regiment.
This retrospective study shows that ATO-ATRA and limited chemotherapy could be a better approach than ATRA and standard intensive chemotherapy in terms of early deaths, LFS and OS.
Disclosures
Heiblig:Jazz Pharmaceuticals: Honoraria; AbbVie: Honoraria; Pfizer Inc.: Honoraria; Astellas: Honoraria; Servier: Honoraria. Bertoli:Novartis: Honoraria; Abbvie: Honoraria, Other: Travel; Astellas: Honoraria; BMS-Celgene: Honoraria; Jazz Pharmaceuticals: Honoraria, Other: Travel; Servier: Honoraria. Cluzeau:Abbvie: Consultancy, Speakers Bureau; Novartis: Consultancy, Speakers Bureau; Incyte: Speakers Bureau; Syros: Speakers Bureau; Jazz Pharma: Consultancy, Speakers Bureau; Servier: Consultancy, Speakers Bureau; Keros: Speakers Bureau; BMS: Consultancy, Speakers Bureau. Raffoux:Pfizer, Inc.: Honoraria; Celgene: Honoraria; AbbVie: Honoraria; Astellas: Honoraria; Daiichi-Sankyo: Honoraria. Fenaux:Jazz: Consultancy, Honoraria, Research Funding; AbbVie: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; French MDS Group: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria, Research Funding. Ades:jazz: Honoraria; Novartis: Consultancy, Research Funding; KEROS: Consultancy; BMS: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding; ROCHE: Honoraria; AMGEN: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal